I've been in the business long enough to remember well those dangerous old scopes used in EIPH diagnosis as pictured above. The new fiber optic models are a vast improvement, but trying to diagnose actual infections in the deepest regions of the lungs is still out of reach of most modern every-day procedures. You can see blood deeper with fiber optics, but you still can't see an lung infection!
Exercise-Induced Pulmonary Hemorrhage or EIPH is one of the major thorns to be encountered in racehorse training and racing. So much so, it is one of the few reasons why state racing commissions will look the other way and allow race-day medication. Lung hemorrhage was actually the cause for me to first become interested in herbal medicine. I was racing at the old AKSARBEN track in Omaha and my horses were suddenly being plagued by bleeding and they were bleeding through their lasix! I was at a loss to know what to do. I knew I had fit horses, so it couldn't be the training. The weather was typical for the Midwest at this time, hot and humid. That was said to contribute toward EIPH. However, no one could give me a reason why EIPH specifically happens with the corresponding veterinary treatments seemingly, hit or miss. What causes it? All the race track vets could do was shrug their shoulders and prescribe the diuretic, Lasix and if that didn't work, they could go underground and give what was known as Kentucky Red ( Carbazochrome Salicylate). Kentucky Red back in the early 1990s was an illegal medication, but it could not be detected. So it was used. Unfortunately it was hard to get and expensive. There had to be a better way! First, it seemed imperative to me to figure out why EIPH happens.
Kenneth W. Hinchcliff of The Ohio State University writes:
"One study examining Thoroughbreds via endoscopy after a single race found that 55% exhibited EIPH to some degree. After following the horses for three races, 85% bled after at least one race. Standardbred racehorses showed a prevalence rate of 87% after at least one of three races." EIPH is widespread and shows no geographic preference. If you do some research online you will find a number of theories on why racehorses bleed. For example, one rather outlandish theory suggests that the impact of the horse's front legs on hard surfaces results in damage to the lung capillaries from the vibration shock which mostly is found to concentrate in the dorsal rear portions of the lungs. Another theory is that during exercise, the horse just naturally produces high blood pressure in the lungs which causes rupture because its heart does not relax quickly enough. Yet others say, some type of upper respiratory obstruction (i.e. recurrent laryngeal neuropathy) could also be involved in stimulating EIPH. Another group suspects that bute (phenylbutazone) may contribute to increasing lung pressures and, thus, bleeding. This leaves the theories of breeders breeding an inferior horse, air pollutants and infections as rounding up the other less commonly heard explanations. Though it is recognized that lung infections could cause bleeding, one really hears very little about pathogens as a cause in most of the EIPH literature. The subject will sometimes be touched upon but it is often shunned as not the major cause, if even a minor one. I say big mistake!
Dr. Paul Ewald and Dr. Gregory Cochran have brought new insight into the field of infectious diseases. Dr. Ewald is a brilliant freethinker, an evolutionary biologist that offers much food for thought when it comes to epidemiology. Before I discuss Ewald, I would like to mention another researcher, Dr. Cochran, who was Dr. Ewald's inspiration. This is all discussed in an exceptional article by Judith Hooper of The Atlantic Monthly . She quotes Dr. Cochran as saying that widespread, old diseases are infectious, if their incidence in the general population is above one-in-one thousand. Likewise, if he sees a disease that has been observed in a population for many years, he becomes very suspicious that it may well be infectious in nature. His view is that the most "fitness antagonistic diseases" must be of an infectious nature as opposed to genetic. The word, "Fitness", is defined as simply the survivability of an animal over others on an evolutionary scale. Judith Hooper writes: "Consider a disease with a fitness cost of one percent -- that is, a disease that takes a toll on survival or reproduction such that people who have it, end up with one percent fewer offspring, on average, than the general population. That small amount adds up. If you have an inherited disease with a one percent fitness cost, in the next generation there will be 99 percent of the original number in the gene pool. Eventually the number of people with the disease will dwindle to close to zero -- or, more precisely, to the rate produced by random genetic mutations: about one in 50,000 to one in 100,000."
This all has major implications to the pathology EIPH of the equine as well. You may ask, how does, say, exercise induced bleeding, affect the fitness of survival/reproduction in our modern racehorse when it seems that most all our racehorses are bred with little effort at culling out race bleeding in our breeding stock? I think this is exactly the key to this question. Bleeding is neither being selected for or against! Thus, it is not realistic to suggest that we are randomly doing exactly that and, additionally, that we are wonderfully successful at achieving increased bleeding in our racehorse population accordingly. It is really hard to breed for a trait. Heritability coefficients can be exceedingly low with success hardly likely even if one is judiciously selecting for it. Only a breeder would appreciate this difficulty. So to make the accusation that our horses are being bred to bleed is ridiculous to me. No one really knows how prevalent bleeding is in our racehorses. There are no accurate statistics and for those that point out that most all of the starters on a card at any race track are on lasix, well, that just means nothing. The mere fact that a horse races on lasix does not confirm a bleeding tendency in the current environment at the American tracks. The first thing, the average American trainer does when a new horse comes into his barn is to get it on lasix as soon as possible. Some states are easier than others in accomplishing this, but any trainer worth his salt can get the job done without ever knowing if his horse is a true bleeder or not. Race track stewards tend to like consistency and having all their horses running on lasix is pretty much a level playing field in their eyes. No wonder lasix is so much abused! I will discuss lasix (furosemide) further, and how it may relate to improving an infection-induced bleeding syndrome. I know there are views that almost all racehorses can be scoped after a race and there will be some bleeding present. Well, I am not really sure what this educated opinion means. Certainly this unsubstantiated opinion has no scientific basis to declaring that most all of our horses are bleeders. The time valued system of breeding the best-to-the-best and hoping-for-the-best, should not in itself be a mechanism to breed our modern thoroughbreds into a bleeding genotype. In short, I would hazard to guess that most all of our bleeding racehorses are suffering from an infection as the work of Dr. Ewald suggests.
So if race bleeding isn't genetic, what is it? Certainly any tendency to bleed in the horse's long ago past would have been bred out by the time that animal evolved up to our current specimens. In prehistoric days, the efficiency of running would have been a life or death trial for selecting the best genes in the primitive horse with bleeding long ago was selected against. I have no reason to believe that somehow our modern racehorses suddenly acquired a genetic defect for bleeding and that this is being selected and perpetuated by our breeders in a random manner. Nonsense! Dr. Ewald's and Cochran's work seem to concur with this hypothesis as well. I say that after considering Ewald and Cochran's bio-evolutionary work, exercise-induced bleeding most probably is highly characteristic of a pathogenic syndrome. It seems so crystal clear to me now after so long puzzling why my horses would occasionally bleed. I knew I sent fit horses to the track--so it couldn't be conditioning. I knew that lasix sometimes helped, but not always. I knew that bleeding was too prevalently seen in a wide diversity of family lines for it to be a genetic thing. Bleeding was seen breed-wide and was historically nothing new. After all, one never goes to the auctions and single out specific family lineage as bleeding prone. It almost has to be environmentally induced, but the question is, what or how? Many people have suggested air pollution could be a reason but, to me, this just didn't make that much sense. A horse was as likely to bleed in the inner foggy city as he was in the crystal clear air of a country track plus pulmonary bleeding accounts could be found in the pre-industrail history. A microorganism cause never seemed to be in question as a general cause of bleeding mainly because bleeding was not obviously infectious by observation or so it seemed. It also did not seem to be affected by common antibiotic therapies, nor could a routine bug be cultured in affected EIPH horses. That is the key! An infection can be an infection without being highly transmissible. The Koch Postulates need not apply! Just because our track and University Vets agree that bleeding is not caused by an infection does not make it so. Just because nothing can be routinely cultured or successfully antibiotically treated does not necessarily exclude a pathogen as a cause.
As of April, 2010 to the best of my knowledge the following should be considered a new theory on equine EIPH which I have formulated. I have yet to find anyone (veterinarian, researcher, and horseman) with a similar theory.
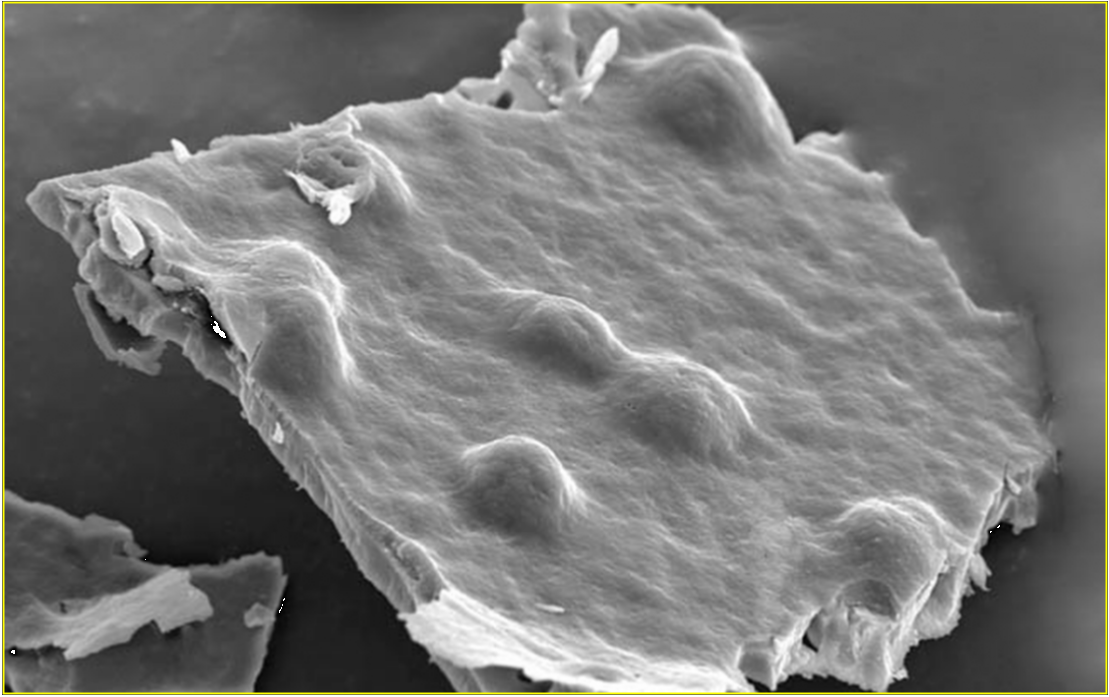
The Ahart Hypothesis: In all likelihood, equine pulmonary bleeding is a symptom of a biofilm infection in the horse's lungs. Biofilms are colonies of bacteria and possibly other microorganism types that have found that living together, protected by a self-secreted polymeric matrix can evade normal immune responses and foster a viable community on a living or non living surface. Dental plaque is probably our best known and studied biofilm which I might add, commonly causes gum bleeding! It is becoming increasingly appreciated that biofilms can be found anywhere in the body. Biofilms are microorganisms characteristically encased by slimy, gluey films that help these pathogenic microorganisms adhere to moist lung tissue and evade the horse's immune cells and commonly administered antibiotics. Biofilms cannot easily be cultured or detected. It is common to inject lasix, a diuretic to treat EIPH in racehorses. It is generally considered that the diuretic effect of Lasix has a direct bearing on lowering plasma volume and reducing right atrial and pulmonary pressure which discourages lung bleeding. Unfortunately, Lasix is not a sure cure and one often has horses bleeding through their lasix on those hot summer days. I would like to suggest another possibility of why Lasix may be therapeutic for EIPH. A study done by Cross, Ramadan, & Thomas, The impact of Furosemide on Pseudomonas Aeruginsoa Biofilms, found that furosemide (lasix) at 10mg/ml reduced some biofilms by 50% at a pH of 8-9. Furosemide seemed to destabilize biofilms at pH-dependent concentrations. Perhaps this is why lasix, generally, but not always, seems to help race track bleeders? It is not so much its diuretic action but rather its biofilm destabilization characteristics that produces efficacy in the bleeding racehorse. Fusomide seems to be only effective at proper pH and specific concentrations which in real life could be quite variable in individual racehorses and racing conditions and may be one reason why we see so much variation in Lasix's efficacy on the track.
It seems quite likely to me that if indeed a biofilm infection is at the heart of our racetrack bleeding problem-that it is in all probability not a simple bacterial biofilm. It could quite likely be made up of a combination of bacteria and fungal components all working in a synergistic environment to further each's goal of survival to the detriment of our racehorse's health. Not only are biofilms off the radar screen of our racetrack vets but a hybrid biofilm consisting of bacteria and fungi would be totally unheard of by this group! Many times, fungi will be secondary colonizers of a biofilm. It has been written that bacteria in these hybrid biofilms can be up to 4000x more resistant to our common antibiotics and the quencher is that common antibiotics have no effect on the fungi found within. A recent study found fungi to be a consistent component in biofilms in sinus mucosal samples from human patients with eosinophilic mucin chronic rhinosinusitis (EMCRS) and allergic fungal rhinosinusitis (AFRS). Why should the equine be much different? Certainly, one of the old time protocols to treating bleeding horses is to be very careful about the hay which is fed, guarding against moldy (fungi infested) hay! Maybe this should be a tip-off of sorts?
A very popular herbal preparation for bleeding is YUNNAN PAIYAO. Many horsemen swear by this Chinese herbal formulation. If you look carefully into its properties, you will find that it contains powerful anti-infective herbs. This clouds up the mechanism of why it seems to help bleeding horses. Is it mostly a blood regulator, anti-hemorrhagic or is it an antibiotic or the combination of the three?
What you will find when you have an infection is that the Vitamin C in the infected region is rapidly utilized and depleted. This holds true for the human who does not synthesize his own Vitamin C as well as the horse that can and does. Infections can and do metabolize huge Vitamin C stores so rapidly in the infected body that a subclinical case of scurvy can be produced in hours. For anyone that has studied scurvy, you know that hemorrhage is the prevalent symptom. Vitamin C is very important in collagen construction and maintenance in blood vessels. Cause a state of depleted Vitamin C and you will have a weakening of collagen structures. Vitamin C is responsible for maintaining iron in its reduced state thereby preserving its numerous iron-containing enzymes which are responsible for the strength and elasticity of blood vessels and capillaries. An interpretation of this phenomena in regard to tuberculosis by Dr. Levy: ". . .a state of focal scurvy exists in the capillaries of affected areas of the lungs. This focal scurvy directly facilitates the rupture of capillaries as they lose their structural integrity, resulting in the coughing up of blood." Though Dr. Levy is describing a tuberculosis infection, the same would hold true for an equine biofilm lung infection. It is not appreciated that pathogens can induce subclinical cases of scurvy! Yes, there is nothing new about the use of Vitamin C and bioflavonoids in the treatment of equine EIPH. Back when I was racing in the early 1980s, one could buy various supplements in the tack shop that contained exactly that for bleeding. Back then, I tended to frown at such an idea. How could "orange juice" possibly help a horse from gushing blood in a race? I didn't appreciate how scurvy was not a disease but a symptom of Vitamin C deficiency and could be found where ever pathogens run riot. I also did not appreciate the fact that dose was everything when it came to Vitamin C which was why Vitamin C often failed. If you do any research on the web, you will find that the veterinary literature will routinely declare that Vitamin C has no proven value in EIPH. This is not surprising, if you want to study the prejudice that has been leveled against Vitamin C since its very inception in the 1930s for the very same reasons. Vitamin C has always been misused and misunderstood. Why should things be any different now? It appears to me that this bias against Vitamin C in regard to EIPH was perpetrated by a a study published in 1984 titled: Exercise-induced pulmonary hemorrhage in Thoroughbred Horses: Response to furosemide or hesperidin-citrus bioflavinoids. There has been no specific studies like this using Ascorbic acid or a similar compound of Vitamin C; so I must only conclude that somehow Hesperidin-citrus bioiflavinoids have been equated with Vitamin C. In this study it was found that neither lasix nor a hesperidins-citrus bioflavonoid product helped bleeding in race horses. This study had a number of built-in flaws which I won't go into, but the results were that 55.7% of the horses treated with lasix still bled. There was no apparent statistical advantage when comparing this treated group from the untreated group. The second study involved treating horses with the bioflavonoid resulting in 84.4% still bleeding resulting in no statistical advantage from the treated to the untreated groups. The oral dosage of the bioflavonoid was 28 grams per day in ration for 90 days. Let me first say, Vitamin C is not a hesperidin-citrus bioflavonoid! You cannot equate the two! Citrus bioflavonoid are found in fruit and their rinds. They are polyphenolic compounds. Vitamin C is a different animal! Secondly, 28 grams daily may not be a proper dose for a biofilm infection. Each individual is different as is its infection. Lastly, this study seemed to show lasix as just as deficient in results as a bioflavonoid, yet the current practice of injecting Lasix has only increased. Go figure?
I might add here that the wide spread use of steroids is very detrimental to the immune system as both the corticosteroids and the anabolics . In our business, it has been all too customary to inject both types of steroids on a routine basis hoping for an edge be it on the race track or just producing a more mature looking yearling. This will open up treated animals to immunosuppressive conditions and presumably make them much more susceptible to biofilm lung infections. Beware of the dangers of such drugs! The key to successfully treating EIPH in the racehorse is to recognize the probable importance of a biofilm infection and treat that infection for what it is-the primary cause. In most cases the common veterinary antibiotics will have little effect on biofilms. Alternative antimicrobial therapies must be utilized that can penetrate the biofilm's protective slime and also treat the fungal component. My book will go into detail how various protocols can successfully eradicate a biofilm infection in the lungs. I will also have herbal formulas in my book where you can make your own bleeder medications that have proven very efficient for my clients and can be seen in the dispensary section of this website. The money you save just from this alone more than justifies the expense of A RACEHORSE HERBAL.
Some of my "THE SPITBOX" message board posts on EIPH may be of interest to you at:
I have partnered with an Irish based herbalist and she has come up with some interesting ideas that may bring another dimension to this problem. She has found my above mentioned hypothesis useful in her practice, but she has come up against particularly difficult-to-treat bleeders that would not respond, if treated specifically for an infection as I suggest. She has come to the conclusion that such horses suffer from DDSP (dorsal displacement of the soft palate), an anatomical/mechanical cause. This is in agreement with Dr. Cook's theory that bleeding is caused by partial asphyxia from DDSP. He has coined a new term, AIPE (asphyxia induced pulmonary edema). He champions the bitless bridle to remedy this problem. His reasons: "The tongue and larynx are joined together anatomically and are both suspended from the skull by the scaffolding of the hyoid bones. Because of this, when the tongue moves, the larynx also moves. If, because of the bit, the tongue moves during galloping, the larynx shifts about like a ship in a storm and this, in turn, interferes with the free passage of air from nose to lung.""If a horse "swallows its tongue'" by evading the bit and draws the tip of its tongue behind the bit, the root of the tongue bulges backward and upward, causing dorsal displacement of the palate (an unbuttoning of the larynx from the soft palate); a folding back of the epiglottis over the mouth of the larynx; a disastrous interference with the flow of air; and a transient episode of suffocation."
"If traction on the bit causes a horse to open its mouth during galloping (or racing), air enters the mouth, from where it may easily rise into the oropharynx (throat). Once this happens, there now being air above and below the soft palate, the soft palate will blow about like a wet sheet in a gale and the horse will make a gurgling noise (or not). Dorsal displacement of the soft palate may well follow. "